The Future of Skin Cancer Detection, Now FDA Cleared.
DermaSensor is more than technology; it is a commitment to helping physicians detect skin cancer at the point of care with the first AI-powered medical device for all three common skin cancers.
Now cleared by the U.S. Food and Drug Administration (FDA), DermaSensor equips physicians with immediate, accurate, and objective results that improve skin cancer detection through data-driven breakthrough technologies.
The Next Chapter in Improved Skin Cancer Detection
Explore functionalities that combine cutting-edge AI technology with non-invasive cancer detection.
Rapid Assessments, Revolutionary AI Technology
Be among the leaders in physician skin cancer lesion assessments and reserve your DermaSensor device for your office today.
Know More. Detect Now.
Set your practice apart by being one of the first primary care physicians in the U.S. to provide non-invasive, point-of-care skin cancer testing. DermaSensor empowers physicians by providing objective, actionable results to aid in skin cancer detection by assessing cellular and sub-cellular features that cannot be seen visually or dermoscopically.
Software Updates
Algorithm Access
Remote Device Monitoring
Validated, AI-Powered

Cloud Storage Access
On Demand Customer Support
See Below the Surface.
Assess cellular and subcellular changes to help primary care physicians better identify skin cancers before they progress.
How it Works
DermaSensor will provide clinicians with additional information about a lesion for them to consider in their referral decision. DermaSensor™ does not definitively determine whether or not cancer is present, specify what type of cancer may be present, nor make any decision for the user.

Identify lesions suggestive of skin cancer on the patient


Five spectral recordings are taken from the skin lesion to complete one scan

Identify lesions suggestive of skin cancer on the patient

Apply handheld DermaSensor device to the lesion and initiate first recording

Five spectral recordings are taken from the skin lesion to complete one scan

DermaSensor’s algorithm analyzes spectral data and delivers assessment in seconds

A result of “Investigate Further” suggests further evaluation through a specialist referral

A result of “Monitor” suggests there is not an immediate need for specialist referral

Technology
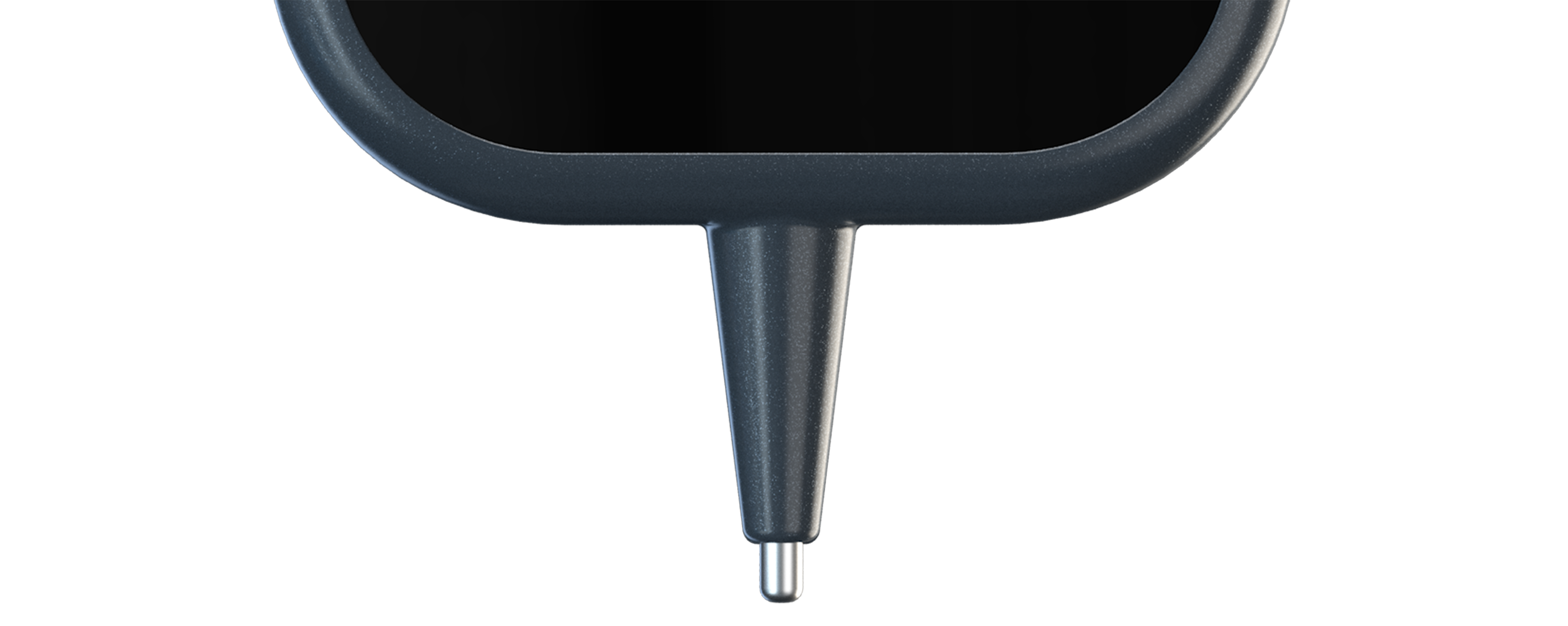
- DermaSensor’s™ tip reflects and records quick bursts of light off the lesion’s cellular and sub-cellular content.
- The light is analyzed by the built-in computer to provide information to help physicians assess skin lesions (including melanomas, squamous cell carcinomas, and basal cell carcinomas) to aid in a referral decision.
- By examining the difference in light scattering, DermaSensor™ determines if the skin lesion is “Investigate Further” or “Monitor,” an immediate output.
- Elastic Scattering Spectroscopy (ESS) has been validated in 30+ publications on clinical studies. Many studies have shown ESS to provide information that is comparable to histopathologic assessment in the analysis of cellular microscopic structure.*
About ESS
DermaSensor™ uses Elastic Scattering Spectroscopy (ESS), a process which evaluates how photons scatter when reflected off of different cellular structures. Malignant lesions have been reported to have different cellular and sub-cellular structures than benign lesions, scattering light differently.

Discover what other practitioners are saying.
Department of Dermatology Clinical Trials Unit
for the DERM-SUCCESS clinical utility study
University of California, San Francisco
Featured In












Spot It First
Secure your spot as a leader in skin cancer detection and healthcare innovation. Elevate your practice with DermaSensor today.
Subscribe To Our Newsletter
80-0009.1 v3
